This post is going to discuss on Iron Metabolism.
Iron is superbly important as it is one of the main constituents of body physiological processes. Below are the lists of iron functions in the body.
Functions
1) Oxygen carriers
+Hemoglobin in red cells
+Myoglobin in myocytes
2) Enzymes in energy production
+Cytochromes (oxidative phosphorylation)
+Krebs cycle enzymes
3) Others
+Liver detoxification through cytochrome P450
Before we go too deep, let us do some simple recap on Chemistry.
Fe2+ – Ferrous (reduced form)
Fe3+ – Ferric (oxidized form)
Fe2+ –> e + Fe3+ (Oxidation process)
e + Fe3+ –> Fe2+ (Reduction process)
Low pH, ferric (3+) reduces into ferrous (2+)
High pH, ferrous (2+) oxidizes into ferric (3+)
Enough with Chemistry, let us get down to on how body absorbs and distributes iron. Before that, let me try to list some terms that you really need to know before we dive deeper into iron metabolism.
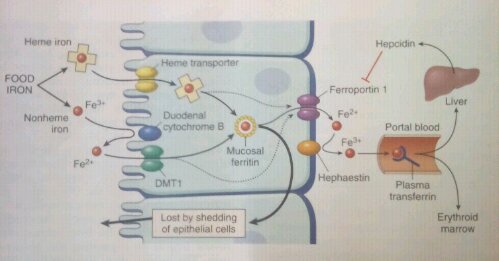
1) DMT1 (Divalent Metal Transporter 1) – A transporter that located in all surfaces of all type of cells in the body, regardless in the GIT or the Endothelial (please be clear on that). So, it can be at the wall of GIT in the lumen, or on the wall of blood vessels. As the name implies, it can only transport Ferrous (Fe2+).
2) Duodenal Cytochome B – A protein having an enzyme called Ferric Reductase on the wall of GIT. Use to reduce ferric (Fe3+) into ferrous (Fe2+).
3) Ferroportin – transporter that transports ferrous (Fe2+) from cells into blood circulation. Located on the surface of cells facing the blood vessel (basolateral membrane)
4) Haphaestin – protein that oxidizes ferrous (Fe2+) into ferric (Fe3+). Located at the surface of cells facing the wall of blood vessels (basolateral membrane)
5) Hepcidin – hepatic peptide; of course released by the liver, use to inhibit the activity of FERROPORTIN. Therefore, increased release of hepcidin, lesser iron will be transported into the blood circulation.
There are few vital proteins involved in distributing iron in the body that we really need to put an attention on it. There are
4) Proteins involved in iron storage
Ferritin
Intracellular protein that binds to ferrous (Fe2+) which acts as the largest form of iron reservoir in the TISSUE. It is called APOFERRITIN when it is not bounded to iron.
Serum ferritin
Regularly, liver and spleen excreted its own ferritin in the blood circulation. It is a vital marker to identify the iron level in the tissue (ferritin) since the value is pretty much the same between both ferritin.
Hemosiderin
Dentured ferritin found in red cells macrophages (Kupffer cells and splenic macrophages). Accumulation of this protein is called as hemosiderosis
Hemoglobin
Protein found in the red cells storing iron in the form of heme
Myoglobin
Protein found the myocytes stroing iron for those cells
5) Protein involved in iron transportation
Transferrin
A protein produced and released by the liver use to transport iron in the form of FERRIC (Fe3+). Transferrin can transport 2irons per molecule of transferrin. Transferrin is also an apoprotein; therefore when in an unbound state it is called as APOTRANSFERRIN
Distribution of iron in the body
Body can only absorb iron in the form of FERROUS only. Why? Cause we only have a Divalent Metal Transporter (DMT1).
Ok, our body absorbs 2 kinds of iron which are:-
1) Heme iron
+ Already in the form of ferrous, therefore readily absorbs by the DMTI
+ Found in the animal liver and beef
2) Non-heme iron
+ In the form of ferric (Fe3+)
+ Found in plant fiber
+ So, it needs to be reduced into ferrous (Fe2+) in order to be absorbed by the DMT1.
At this state, Duodenal Cytochrome B plays its important role by reducing ferric (Fe3+) into ferrous (Fe2+) using its enzyme called Ferric Reductase.
When all iron are in the reduced form (Fe2+), it will then transported into the enterocytes (cells of the GIT) through DMT1. At this point, ferrous (Fe2+) got 2 fates, which either
1) Stored in the enterocytes in the form of iron ferritin OR
2) Transported to other tissues; importantly erythroid tissue of the red marrow in the form of transferrin.
So, let us discuss on how iron is transported to the other tissues
We already know that all iron in the enterocytes are in the reduced form (Fe2+) but transferrin can only bind to FERRIC (Fe3+).Ting Tong!! So how does body work this thing out? We have Haphaestin, a protein that is used to oxidize the ferrous (Fe2+) into ferric (Fe3+). Haaa, what a relief!! =D
Once it is oxidized, ferric (Fe3+) will bind to transferrin and it will be transported into tissues that need it especially erythroid tissue of the red marrow.
Above of all of these mechanisms, there is a peptide released by the liver which controls the metabolism of iron in the body; Hepcidin. Hepcidin is used to inhibit the action of ferroportin; therefore increased hepcidin release will reduce iron transport outside the cells.
Enough with that, let us discuss on how cell gets iron from transferrin.
1) Transferrin with 2 irons will bind to transferrin receptor on the surface of a cell. Ok, let us called it as Transferrin-Receptor Complex (TRC).
2) TRC is then transported into the cell through a vesicle. The process is called as Receptor Mediated Endocytosis.
3) Ion pumps (H+-ATPase) will reduce the pH inside the vesicle so that Fe3+ will be reduced into Fe2+ so that the iron is not fit to the transferrin anymore and will be released into the vesicle.
4) Fe2+ is then transported into the cell cytoplasm through the DMT1 which is also inside the vesicle.
5) The TRC is transported back outside the cell to be recycled.
I hope this post could help you a little bit in order to understand the pathology of iron deficiency anemia and also pharmacology basis of iron therapy
With that thanks guys!!